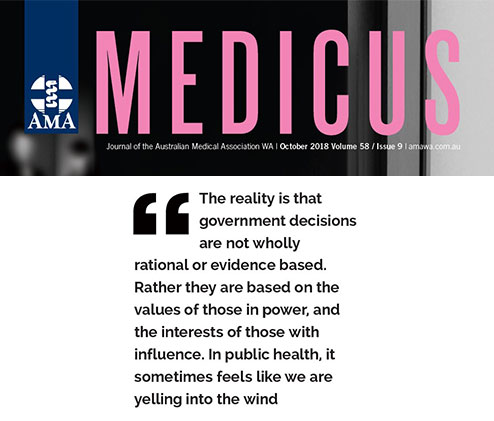
The Australian Medical Association (WA) Blog showcases a range of commentary, opinion pieces, profiles and insightful features – all designed to educate, inform and yes, in some cases, even entertain.
The AMA (WA) Blog can be accessed by members, all other healthcare professionals and the general public.