
Blog
Flashback Friday: How Healthy is Rural Health? – November 2012
Friday November 19, 2021
The key issue of rural health has been in the news of late and not in a positive manner.
Doctors leaving the Goldfields, key services such as obstetrics in some country centres being closed by the Health Department, and staff shortages across the board have all served to focus attention on how health services are provided to the almost one million people who live outside the Perth metropolitan area.
Everyone would agree that the quality of health delivery is a key measure of our standing as a modern first-world state and yet there are a number of questions being asked regularly about the health of health services in WA.
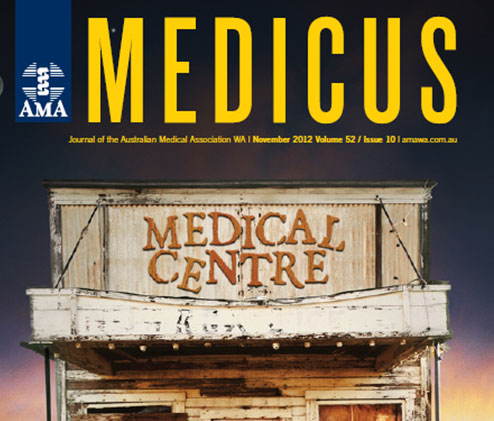
As an example, Laverton Hospital hit the headlines last month for all the wrong reasons. Forty years since its last renovation, the ageing medical centre which services the small WA Goldfield’s town – almost 1000km north-east from Perth – was reported to be in desperate need of repair and redevelopment.
Concerns about the state of the facility were even raised in Parliament by Pastoral and Mining MLC, Wendy Duncan. The inventory of complaints covered everything from insufficient toilets, substandard sewage, roof leaks and even the presences of asbestos in the construction – never mind the disregard of occupational health and safety regulations and emergency patients being wheeled through the rear, as the front entrance cannot accommodate modern ambulances. A new ramp has only just been constructed at the front of the building.
Councillor Patrick Hill from Laverton Shire said the condition of the hospital was appalling and residents have long been crying out for some form of acknowledgement backed by concrete action. Both Ms Duncan and Councillor Hill have put together two petitions, both supported strongly by Laverton residents, and local Aboriginal and mining communities, calling on the government to build a multi-purpose health facility in Laverton that will serve patients as well as offer ancillary health services.
Reports on the plight of Laverton Hospital have, as expected, turned up the heat on the condition of public health services in regional and remote WA and in particular, the crucial shortage of medical practitioners and generalist doctors. Certainly, the issues are far too complex to unearth a simple solution.
Medicus asked a panel of medical practitioners, educationists and Councillor Hill about their experiences in regional WA, their growing concerns about health services in their beloved town, their visions for the future and their suggestion for possible solutions.
“The current design of the hospital is out-dated and inadequate for demands and expected services,” – Patrick Hill, Councillor, Shire of Laverton.
“To respond to the initial challenge of identifying a workforce, we need “generalist” specialists. The ones we have are perilously close to retirement and irreplaceable at present. There just isn’t enough work out here for sub-specialists. Visiting specialists are great but we do need someone in town for the acute issues. Next, we need GP proceduralists. We don’t need a huge number as (for better or worse) the big towns don’t need them as much now and only a few small towns have hospitals. But in those key procedural small towns, the procedural GPs are absolutely critical to the survival of obstetrics and emergency services. Lastly, we need a good solid GP service to look after chronic illness, aged care, paediatrics and more,”- Dr Peter Maguire.
“Small rural hospitals are also on the agenda nationally, mainly regarding the funding model. It is obvious to us, but not necessarily to accountants or bureaucrats, that funding formulae for small hospitals can’t be the same as for RPH or SCGH. There is a real risk that funding to small hospitals may be squeezed by the application of inappropriate financial models,”- Dr Peter Maguire.
“The solution to the rural medical workforce problem is complex. Rural selection quotas, exposure and training programs in Australian medical schools are just one part of the solution. All Australian medical schools are required to reserve 25 per cent of admissions for rural origin students,” – Winthrop Professor Geoff Riley.

